Is Natural Immunity More Effective Than the COVID-19 Shot?
According to Centers for Disease Control and Prevention data, COVID-19 “cases” have trended downward since peaking during the first and second week of January 2021.
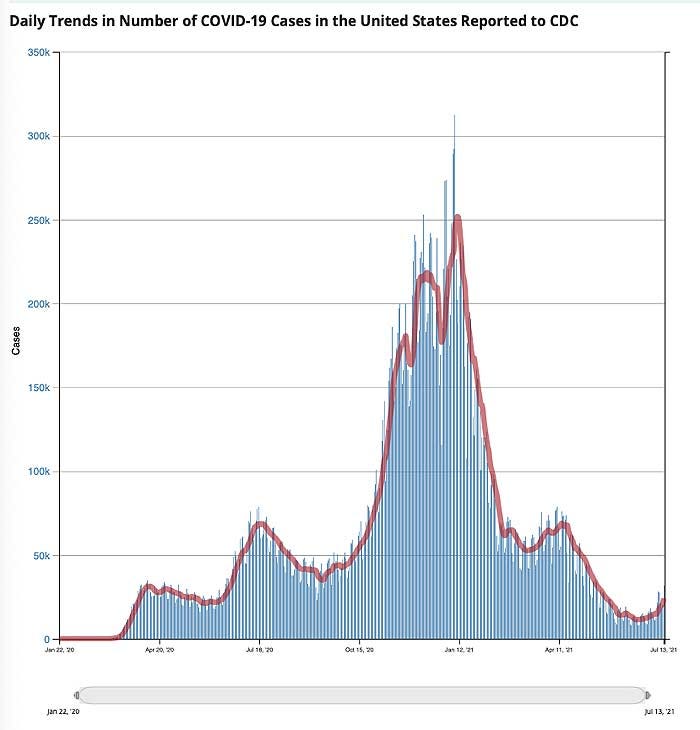
At first glance, this decline appears to be occurring in tandem with the rollout of COVID shots. January 1, 2021, only 0.5% of the U.S. population had received a COVID shot. By mid-April, an estimated 31% had received one or more shots, and as of July 13, 48.3% were fully “vaccinated.”
However, as noted in a July 12, 2021, STAT News article,“cases” had started their downward trend before COVID shots were widely used. “Following patterns from previous pandemics, the precipitous decline in new cases of Covid-19 started well before a meaningful number of people had been vaccinated,” Robert M. Kaplan, Professor Emeritus at the UCLA Fielding School of Public Health, writes. He continues:
...
As noted by Kaplan, COVID-19 “cases” peaked in early January 2021. January 8, more than 300,000 new positive test results were recorded on a daily basis. By February 21, that had declined to a daily new case count of 55,000. COVID-19 vaccine injections were granted emergency use authorization at the end of December 2020, but by February 21, only 5.9% of American adults had been fully vaccinated with two doses.
Despite such a low vaccination rate, new “cases” had declined by 82%. Considering health authorities claim we need 70% of Americans vaccinated in order to achieve herd immunity and stop the spread of this virus..
...
As noted by Kaplan, the most reasonable explanation for declining rates of SARS-CoV-2 appears to be natural immunity from previous infections, which vary considerably from state to state. He goes on to cite a study by the National Institutes of Health, which suggests SARS-CoV-2 prevalence was 4.8 times higher than previously thought, thanks to undiagnosed infection.
...
Vaccine Provides Far Less Protection Than Natural Immunity
While some claim vaccine-induced immunity offers greater protection against SARS-CoV-2 infection than natural immunity, historical and current real-world data simply fail to support this assertion.
As recently reported by Attkisson and David Rosenberg Israeli National News, recent Israeli data show those who have received the COVID jab are 6.72 times more likely to get infected than people who have recovered from natural infection.
Among the 7,700 new COVID cases diagnosed so far during the current wave of infections that began in May 2021, 39% were vaccinated (about 3,000 cases), 1% (72 patients) had recovered from a previous SARS-CoV-2 infection and 60% were neither vaccinated nor previously infected.
...
Natural Immunity Appears Robust and Long-Lasting
An argument we’re starting to hear more of now is that even though natural immunity after recovery from infection appears to be quite good, “we don’t know how long it’ll last.” This is rather disingenuous, seeing how natural immunity is typically lifelong, and studies have shown natural immunity against SARS-CoV-2 is at bare minimum longer lasting than vaccine-induced immunity.
Here’s a sampling of scholarly publications that have investigated natural immunity as it pertains to SARS-CoV-2 infection. There are several more in addition to these:
According to Centers for Disease Control and Prevention data, COVID-19 “cases” have trended downward since peaking during the first and second week of January 2021.
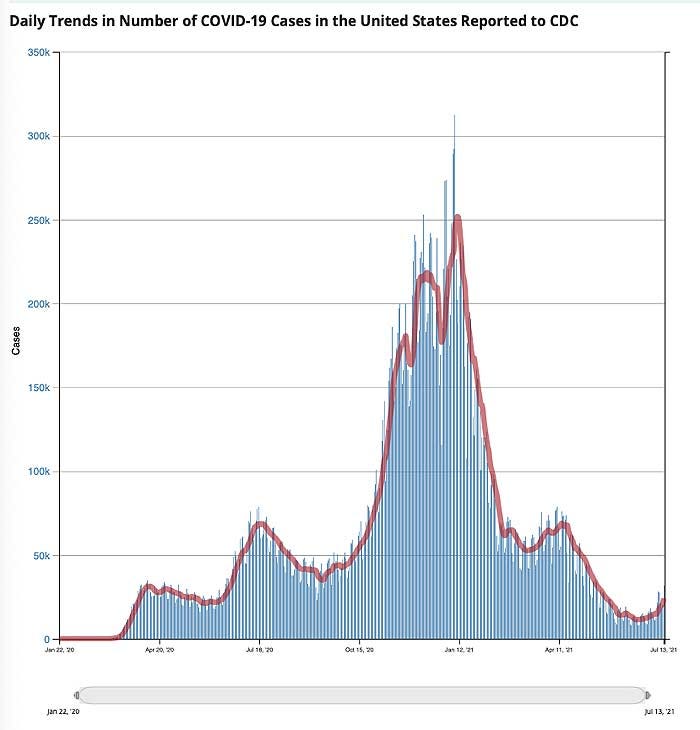
At first glance, this decline appears to be occurring in tandem with the rollout of COVID shots. January 1, 2021, only 0.5% of the U.S. population had received a COVID shot. By mid-April, an estimated 31% had received one or more shots, and as of July 13, 48.3% were fully “vaccinated.”
However, as noted in a July 12, 2021, STAT News article,“cases” had started their downward trend before COVID shots were widely used. “Following patterns from previous pandemics, the precipitous decline in new cases of Covid-19 started well before a meaningful number of people had been vaccinated,” Robert M. Kaplan, Professor Emeritus at the UCLA Fielding School of Public Health, writes. He continues:
“Nearly 50 years ago, medical sociologists John and Sonja McKinlay examined death rates from 10 serious diseases: tuberculosis, scarlet fever, influenzae, pneumonia, diphtheria, whooping cough, measles, smallpox, typhoid, and polio. In each case, the new therapy or vaccine credited with overcoming it was introduced well after the disease was in decline.
More recently, historian Thomas McKeown noted that deaths from bronchitis, pneumonia, and influenza had begun rapidly falling 35 years before the introduction of new medicines that were credited with their conquest. These historical analyses are relevant to the current pandemic.”
More recently, historian Thomas McKeown noted that deaths from bronchitis, pneumonia, and influenza had begun rapidly falling 35 years before the introduction of new medicines that were credited with their conquest. These historical analyses are relevant to the current pandemic.”
...
As noted by Kaplan, COVID-19 “cases” peaked in early January 2021. January 8, more than 300,000 new positive test results were recorded on a daily basis. By February 21, that had declined to a daily new case count of 55,000. COVID-19 vaccine injections were granted emergency use authorization at the end of December 2020, but by February 21, only 5.9% of American adults had been fully vaccinated with two doses.
Despite such a low vaccination rate, new “cases” had declined by 82%. Considering health authorities claim we need 70% of Americans vaccinated in order to achieve herd immunity and stop the spread of this virus..
...
As noted by Kaplan, the most reasonable explanation for declining rates of SARS-CoV-2 appears to be natural immunity from previous infections, which vary considerably from state to state. He goes on to cite a study by the National Institutes of Health, which suggests SARS-CoV-2 prevalence was 4.8 times higher than previously thought, thanks to undiagnosed infection.
...
Vaccine Provides Far Less Protection Than Natural Immunity
While some claim vaccine-induced immunity offers greater protection against SARS-CoV-2 infection than natural immunity, historical and current real-world data simply fail to support this assertion.
As recently reported by Attkisson and David Rosenberg Israeli National News, recent Israeli data show those who have received the COVID jab are 6.72 times more likely to get infected than people who have recovered from natural infection.
Among the 7,700 new COVID cases diagnosed so far during the current wave of infections that began in May 2021, 39% were vaccinated (about 3,000 cases), 1% (72 patients) had recovered from a previous SARS-CoV-2 infection and 60% were neither vaccinated nor previously infected.
...
Natural Immunity Appears Robust and Long-Lasting
An argument we’re starting to hear more of now is that even though natural immunity after recovery from infection appears to be quite good, “we don’t know how long it’ll last.” This is rather disingenuous, seeing how natural immunity is typically lifelong, and studies have shown natural immunity against SARS-CoV-2 is at bare minimum longer lasting than vaccine-induced immunity.
Here’s a sampling of scholarly publications that have investigated natural immunity as it pertains to SARS-CoV-2 infection. There are several more in addition to these:
- Science Immunology October 2020 found that “RBD-targeted antibodies are excellent markers of previous and recent infection, that differential isotype measurements can help distinguish between recent and older infections, and that IgG responses persist over the first few months after infection and are highly correlated with neutralizing antibodies.”
- The BMJ January 2021 concluded that “Of 11, 000 health care workers who had proved evidence of infection during the first wave of the pandemic in the U.K. between March and April 2020, none had symptomatic reinfection in the second wave of the virus between October and November 2020.”
- Science February 2021 reported that “Substantial immune memory is generated after COVID-19, involving all four major types of immune memory [antibodies, memory B cells, memory CD8+ T cells, and memory CD4+ T cells]. About 95% of subjects retained immune memory at ~6 months after infection. Circulating antibody titers were not predictive of T cell memory.Thus, simple serological tests for SARS-CoV-2 antibodies do not reflect the richness and durability of immune memory to SARS-CoV-2.” A 2,800-person study found no symptomatic reinfections over a ~118-day window, and a 1,246-person study observed no symptomatic reinfections over 6 months.
- A February 2021 study posted on the prepublication server medRxiv concluded that “Natural infection appears to elicit strong protection against reinfection with an efficacy ~95% for at least seven months.”
- An April 2021 study posted on medRxiv reported “the overall estimated level of protection from prior SARS-CoV-2 infection for documented infection is 94.8%; hospitalization 94.1%; and severe illness 96·4%. Our results question the need to vaccinate previously-infected individuals.”
- Another April 2021 study posted on the preprint server BioRxiv concluded that “following a typical case of mild COVID-19, SARS-CoV-2-specific CD8+ T cells not only persist but continuously differentiate in a coordinated fashion well into convalescence, into a state characteristic of long-lived, self-renewing memory.”
- A May 2020 report in the journal Immunity confirmed that SARS-CoV-2-specific neutralizing antibodies are detected in COVID-19 convalescent subjects, as well as cellular immune responses. Here, they found that neutralizing antibody titers do correlate with the number of virus-specific T cells.
- A May 2021 Nature article found SARS-CoV-2 infection induces long-lived bone marrow plasma cells, which are a crucial source of protective antibodies. Even after mild infection, anti-SARS-CoV-2 spike protein antibodies were detectable beyond 11 months’ post-infection.
- A May 2021 study in E Clinical Medicine found “antibody detection is possible for almost a year post-natural infection of COVID-19.” According to the authors, “Based on current evidence, we hypothesize that antibodies to both S and N-proteins after natural infection may persist for longer than previously thought, thereby providing evidence of sustainability that may influence post-pandemic planning.”
- Cure-Hub data confirm that while COVID shots can generate higher antibody levels than natural infection, this does not mean vaccine-induced immunity is more protective. Importantly, natural immunity confers much wider protection as your body recognizes all five proteins of the virus and not just one. With the COVID vaccine, your body only recognizes one of these proteins, the spike protein.
- A June 2021 Nature article points out that “Wang et al. show that, between 6 and 12 months after infection, the concentration of neutralizing antibodies remains unchanged. That the acute immune reaction extends even beyond six months is suggested by the authors’ analysis of SARS-CoV-2-specific memory B cells in the blood of the convalescent individuals over the course of the year.These memory B cells continuously enhance the reactivity of their SARS-CoV-2-specific antibodies through a process known as somatic hypermutation. The good news is that the evidence thus far predicts that infection with SARS-CoV-2 induces long-term immunity in most individuals.”
- Another June Nature paper concluded that “In the absence of vaccination antibody reactivity [to the receptor binding domain (RBD) of SARS-CoV-2], neutralizing activity and the number of RBD-specific memory B cells remain relatively stable from 6 to 12 months.” According to the authors, the data suggest “immunity in convalescent individuals will be very long lasting.”
